Capacitive hyperthermia in combination with palliative radiation therapy of painful bony metastases
Capacitive hyperthermia can enhance the effectiveness of radiotherapy
Palliative-analgesic radiotherapy is a frequently employed treatment for painful bony metastases. However, only approximately one third of affected patients experiences pain relief from radiotherapy alone, and only a quarter reports complete pain relief. When hyperthermia, i.e. heating the tissue to approximately 40°C to 43°C, is used as a supplementary treatment, it can enhance the effectiveness of radiotherapy. Heating the tissue not only interferes with DNA repair mechanisms, but also ensures a larger oxygen supply for tumors due to improved circulation. Capacitive hyperthermia relies on a plate capacitor, the simplest method to generate heat via an electromagnetic field.
Positive data on capacitive hyperthermia are available from randomized studies on cervical cancer, ear, nose and throat tumors, and esophageal cancer. Since this technology is also suitable for local hyperthermia, which is typically performed with microwave applicators, the positive randomized studies on local hyperthermia – for example, on metastatic melanoma or recurrent breast cancer – are applicable in the same manner as capacitive hyperthermia. Little was previously known on the combination of capacitive hyperthermia and radiotherapy for the treatment of painful bony metastases.
Randomized phase-III study
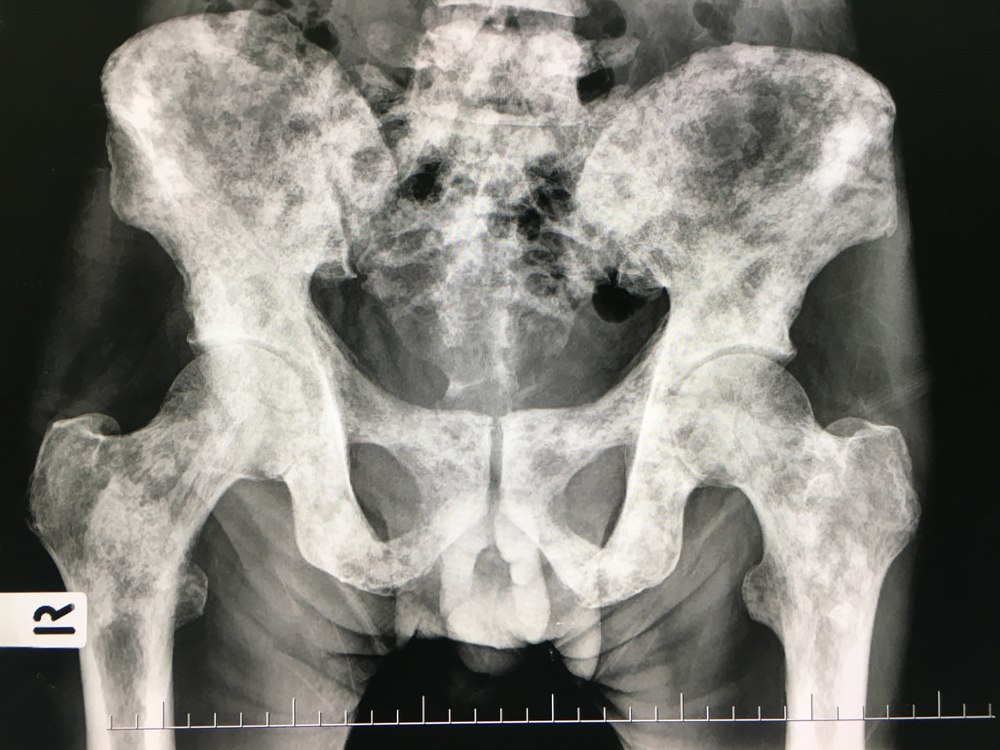
A randomized phase-III study compared the effectiveness of combined capacitive hyperthermia and radiotherapy with radiotherapy alone to evaluate the difference in pain reduction in patients suffering from painful bony metastases. The primary endpoint was the number of patients with complete pain relief at a predetermined site (index lesion) within 3 months after radiotherapy, defined as a BPI (Brief Pain Inventory) score of 0 without increasing the previously existing pain medication. Secondary endpoints included the time and duration of complete pain relief, treatment-related adverse events, and differences in the radiological tumor response. Patients enrolled in the study had solid tumor bony metastases and a life expectancy of at least 3 months. The index lesion was defined as a lesion < 20 cm with a BPI score of at least 4, and had to effectively be covered by electrodes with a maximum diameter of 30 cm. Although each patient could only have one index lesion, radiation to additional lesions was permitted. The strength of other systemic therapy and analgesics was to remain unchanged for 4 weeks before and during the radiotherapy. Exclusion criteria included pathological fractures, lesions of the skull, a history of metal implants such as cardiac pacemakers, and previous radiation to the lesion site. The affected patients were stratified by the number of bony metastases – solitary versus multiple –, by primary tumor type – prostate cancer as well as breast cancer versus other tumors –, and BPI score – 4-6 versus 7-10 points. The radiotherapy was administered for 2 weeks with 5 fractions per week, either using intensity-modulated radiotherapy or 3D-conformal radiotherapy.
The hyperthermia was administered to patients in supine position, twice weekly, for a total of four times, using the capacitive technology of the Thermotron-RF8 system. This treatment occurred within 2 hours after radiotherapy with the target temperature remaining consistent for 40 minutes. In most cases, no invasive temperature measurement was performed. The BPI was measured 15 times during the six-month follow-up phase. Hyperthermia-related adverse events were recorded with the Common Terminology Criteria for Adverse Events, Version 4.0. The radiological response was evaluated 3 months after the treatment, using computed tomography and the Response Evaluation Criteria in Solid Tumors, Version 1.1.
After a planned interim analysis, the study was terminated early 3 years after its start, with an enrollment of 57 patients (29 patients whose treatment involved a combination of hyperthermia and radiotherapy, 28 patients treated with radiotherapy only) since the primary endpoint showed a significant outcome in favor of the combination treatment. Because of the slow recruitment, more than another 3 years would have been required to enroll the initially projected sample of 152 patients.
Study results
Complete pain relief within 3 months after the treatment was 58.6% in the combined hyperthermia and radiotherapy group and 32.1% in the radiotherapy-alone group. When radiotherapy was applied alone, the median time to pain progression was 55 days for patients with complete pain relief. This endpoint was not reached in the combination arm. The non-accumulated rate of complete pain relief 3 months after the treatment was 37.9% in the combination arm and 7.1% with radiotherapy alone. In addition, a significantly higher rate of radiological response was determined in patients who had been treated with combined radiotherapy and hyperthermia than in those who had only received radiotherapy (73.4% versus 25%). Eight patients (53.3%) showed at least partial new bone formation in the combination treatment. This was only the case in 2 patients (16.7%) after radiotherapy treatment alone. The adverse events in both study types were minor; no grade 3 adverse events were reported. In the combination arm, local heat-related pain was reported more frequently, and a subcutaneous fat induration persisting for several weeks was observed in obese patients.
Discussion
As a result, it can be established that the rate of complete pain relief 3 months after analgesic palliative radiotherapy with 10 x 3 Gy increases significantly if capacitive hyperthermia treatment is administered in addition to radiotherapy. The median time to pain progression was also significantly longer after the combination therapy compared to the sole application of radiotherapy. The study was terminated early after the performance of the planned interim analysis, both for reasons of slow patient recruitment and due to the significant difference in complete pain relief after 3 months, which was clearly in favor of capacitive hyperthermia. This was considered the clinically relevant final result and withholding hyperthermia was even considered unethical.
It is noteworthy in this context that the rate of full pain relief 3 months after exclusive radiotherapy was comparatively low with 7.1%. It is conceivable that this was associated with certain characteristics of the patients enrolled in the study, in whom advanced bony metastases with soft tissue involvement may have been present more frequently without any information provided in the publication. This may also explain the additional high benefit of hyperthermia since soft-tissue lesions can generally be heated up more easily than is the case with bony lesions. Such bony lesions with a higher proportion of soft tissue may be more effective to treat with higher radiation doses.
Capacitive hyperthermia ranks between local and regional hyperthermia with regard to achievable penetration depth. A number of different frequencies can be applied, for example 8 MHz in Asia with the Thermotron system used in this case or the approved ISM frequency of 13.56 MHz, for example with the capacitive devices of Celsius42 GmbH, which are widely used in Europe and specifically Germany. Although capacitive hyperthermia is relatively easy to administer and is well tolerated by patients, the achieved temperature distributions are only satisfactory with certain parameters. A homogeneous electromagnetic field can only be established between the two electrodes if the dimensions of the electrodes are ideally much larger than the distance between the two poles. However, this cannot always be achieved in the human body based on the region and physical properties.
The largest obstacle to achieving a satisfactory heat distribution with capacitive hyperthermia in fact is the inhomogeneity of the human body, which is based on larger bone sections and layers of fat, but primarily on air. As the electrically thinner medium, fat can show unwanted overheating at the surface, which in part can only be prevented by cooling the surface.
In the study results, the relatively lean body appearance of Asian patients should be taken into account in addition to patient selection. As a result, the results may only be transferable to a limited extent to central Europeans, who typically have a higher average BMI. It is therefore recommended to perform a study in Germany to confirm the above-referenced results with consideration for higher radiation doses for lesions with a soft-tissue proportion to gain further evidence of the significance of hyperthermia in conjunction with palliative radiotherapy.
Final findings
It can be presumed that the combination of capacitive hyperthermia and palliative radiotherapy is superior to the sole application of radiotherapy in terms of pain relief after 3 months. Similar results can be postulated for the application of regional hyperthermia. Nevertheless, there are still open questions, for example with regard to hyperthermia technique and patient selection. It is therefore recommended to perform additional studies on the topic because Germany offers favorable conditions for treating the affected patients and for future studies.
(This text is based on an article by Pirus Ghadjar, Peter Wust and Volker Budach, Berlin as well as Wilfried Budach, Düsseldorf and their article published by Springer Verlag).
